Does Medicare Pay For Purewick
Medicare may also cover a catheter if your urinary incontinence or urinary retention is determined to be permanent or lasting three or more months. 1).they are distinguished from indwelling catheters that are inserted into the bladder vesicle using a transurethral or suprapubic route.

Nahc Receives Clarification On Coverage For The Purewick System Nahc Report
Medicare offers coverage for all types of urinary catheters and drainage bags through both original medicare and medicare advantage plans.

Does medicare pay for purewick. Part a deductible the medicare part a deductible is $1,364 per benefit period in 2019. Usually doesn’t cover common medical supplies, like bandages and gauze, which you use at home. Medicare part b (medical insurance) part b covers certain doctors' services, outpatient care, medical supplies, and preventive services.
The system is $800 to get with cash only, and then it's $500 a month after that for the external catheters. Purewick is now covered by medicare. My mom was so excited to get her purewick urinary collection system, but as of this week, medicare no longer covers it.
It draws urine away to keep skin dry and control odor. How often do you change purewick? Find your best rate from over 4,700 medicare plans nationwide.
Medicare statute and regulations allow for payment on either a rental or purchase basis for this equipment, but total payments cannot exceed the medicare purchase price for the equipment. The prosthetic device benefit (social security act 1861 (s)(8)) covers urological supplies. The system contains five components as.
Get info on what is covered through your plan on medicare.gov. Protect the best years ahead. Updated on september 28, 2021.
Until national medicare coverage and payment guidelines have been established for these codes, the medicare coverage and payment determinations for these items may be made based on the discretion of the macs processing claims for these items. The type of facility may also determine what benefits are available. Medicare pays 80% of your intermittent catheter supply cost after the annual deductible is met.
Payment on the grounds that its contract calls for medicare to pay first. Hcpcs codes effective october 1, 2020. A three way indwelling catheter either alone(a4346) or with other components (a4313 or a4316) will be covered only if
Ad shop 2020 medicare plans. Medicare covers catheters and related medical supplies that a doctor says is medically necessary. This itemis identified by code k0554 in the hcpcs.
If your home health agency doesn’t supply durable medical equipment directly, the home health agency staff will usually arrange for a home equipment supplier to bring Find your best rate from over 4,700 medicare plans nationwide. If you have medicare and a secondary insurance plan, the supplemental insurance will most likely cover the remaining 20% of the supply cost.
Coverage depends on the type of catheter and the medical reason for it. Must meet certain criteria and be ordered by a doctor. Generally, the beneficiary is not disadvantaged where medicare is the secondary payer because the
Additionally, your physician must deem it to be medically necessary to have the catheter , and you must have. 23.8%, representing a projected improper payment amount of approximately $70,873,477 million. If, after the primary payer processes the claim, it does not pay in full for the services, medicare secondary benefits may be paid for the services as prescribed in §10.8.
Protect the best years ahead. The urinary (foley) catheter is placed into the bladder through the urethra, the opening through which urine passes. How much does a catheter cost with medicare?
Medicare covers some supplies as durable medical equipment. Benefits also include catheter supplies like irrigation kits, bedside drain. Ad shop 2020 medicare plans.
What holds a urinary catheter in place? Under the local coverage determinations for external infusion pumps (l33794), medicare only Catheters may be covered as prosthetics if you have a permanent condition.
Does medicare pay for purewick? If documentation is requested and does not substantiate medical necessity payment for a4340, a4344, a4312, or a4315 will be denied as not reasonable and necessary. The dme macs and a/b macs part b shall establish local fee schedule
Incontinence supplies coverage and adult diapers are not available through medicare. Thereof, what does medicare pay for catheters? Substantiate medical necessity payment for a4340, a4344, a4312, or a4315will be denied as not reasonable and necessary.
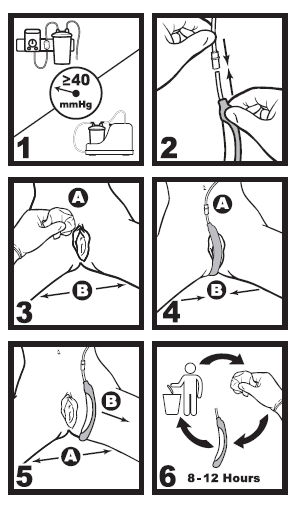
External collection devices are defined as a category of devices that adhere to the external genitalia or pubic area and collect urinary output (figure (figure1). A three way indwelling catheter either alone (a4346) or with other components (a4313 or a4316) will be covered only if continuous catheter irrigation is reasonable and necessary.

Bard Purewick Female External Catheter Pwf030 Vitality Medical

Purewick System
How To Use Purewick

Buy Purewick Female External Catheter Online In Indonesia B07zfxctrs

Does Medicare Cover Catheters - What Types Are Covered - Medicarefaq

Purewick Liberator Medical

The Purewick Tv Commercial Wake Up Dry Covered By Medicare - Ispottv

Purewick Liberator Medical

The Purewick Tv Commercial Wake Up Dry Covered By Medicare - Ispottv

Purewick Liberator Medical

Ways To Pay

Purewick Female External Catheter Shop Purewick Catheter
Kaybee - Wackywednesday Brings You The Bd Purewick Facebook

The Purewick Tv Commercial Wake Up Dry Covered By Medicare - Ispottv

The Purewick Tv Commercial Wake Up Dry Covered By Medicare - Ispottv

Does Medicare Pay For Purewick - Cement Answers

Purewick Female External Catheter

Purewick Liberator Medical

How It Works